DIABETIC EYE DISEASE
High blood sugar levels in patients with diabetes can damage blood vessels in the retina, the thin layer of nerve fibers in the back of the eye that senses light. Damage to retinal blood vessels is referred to as diabetic retinopathy. There are two types of diabetic retinopathy, non-proliferative and proliferative. Non-proliferative diabetic retinopathy is commonly referred to as background retinopathy. In this stage tiny blood vessels within the retina leak blood and fluid. Vision may not be affected at all in this early stage. When vision is affected it is usually the result of macular edema and or macular ischemia.
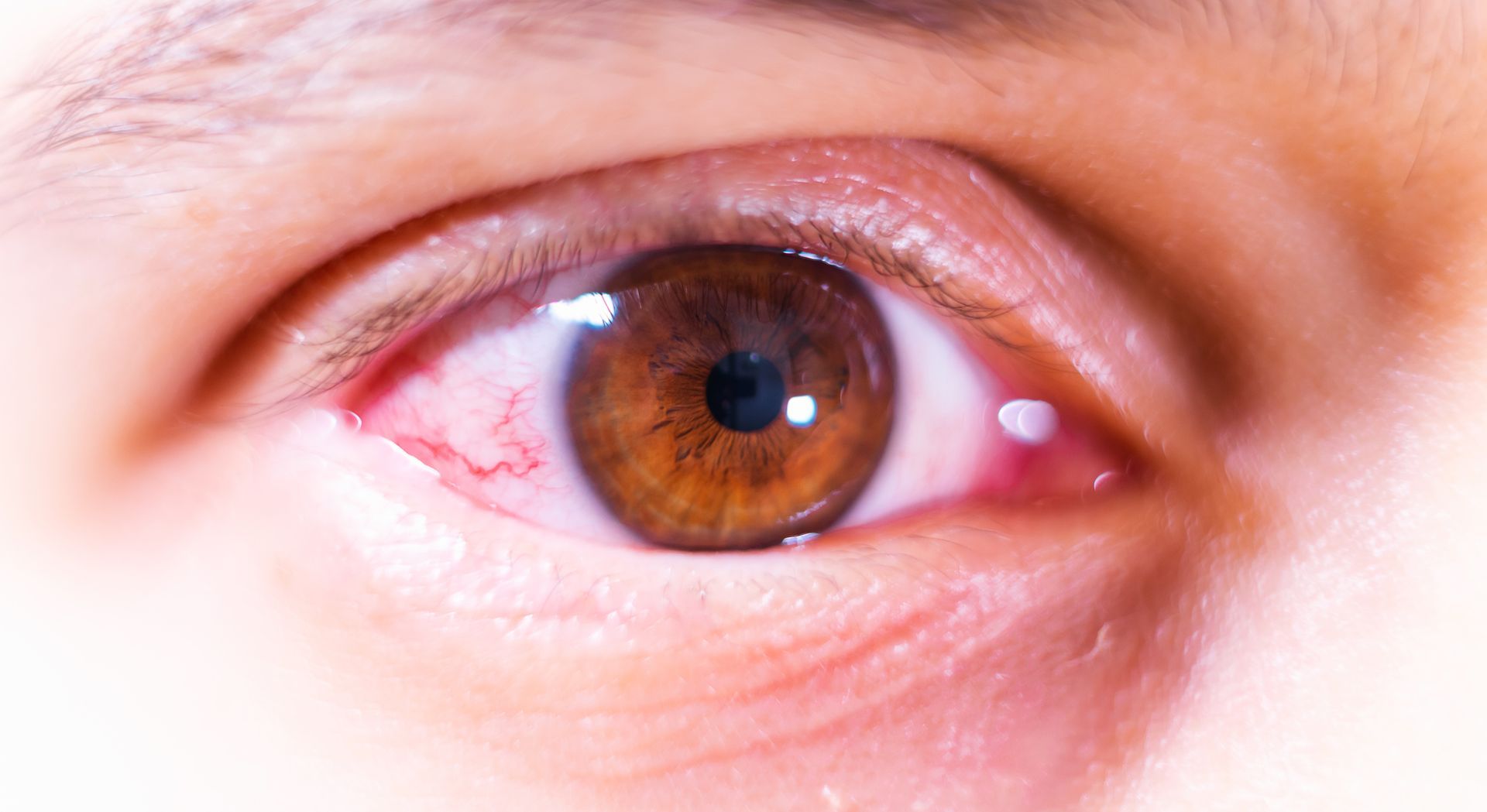
Macular edema is swelling or thickening of the macula, a small area in the center of the retina that allows us to see fine detail clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Macular ischemia occurs when small blood vessels close. The vision blurs because the macula no longer receives enough blood supply to work properly.
Proliferative diabetic retinopathy occurs when abnormal blood vessels grow on the surface of the retina or optic nerve. The retina responds by growing more abnormal blood vessels in attempt to supply blood to the area where the original vessels closed. Unfortunately, these abnormal blood vessels are not effective at resupplying the retina with normal blood flow and are often accompanied by scar tissue that causes wrinkling or detachment of the retina. Additionally the fragile abnormal new blood vessels may bleed into the vitreous cavity of the eye. This is known as a vitreous hemorrhage and the blood can block the vision and may take days or months to clear. If the eye does not clear the blood from the vitreous within a reasonable time, vitrectomy surgery with removal of the blood may be recommended.
Medical eye examinations are the best way to detect diabetic eye disease. Following pupil dilation, Dr. Jones will look in your eyes with special equipment and lenses. Florescein angiography and OCT testing are common technologies we use to evaluate diabetic retinopathy.
The best treatment is to prevent the development of diabetic retinopathy as much as possible with excellent control of blood sugars. Control of high blood pressure and kidney issues are also important. Medical treatment with anti-VEGF and steroid injections can reduce swelling of the macula and improve vision. Laser treatment is often used to shrink abnormal blood vessels with proliferative retinopathy.
BROWSE OUR WEBSITE
CONTACT INFORMATION
1951 Bench Road – Suite C Pocatello, ID 83201
- Mon - Thu
- -
- Friday
- -
- Sat - Sun
- Closed